









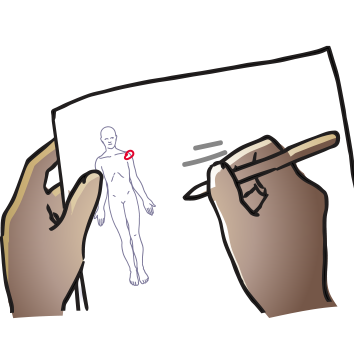
S.O.A.P. notes make your assessment and treatment logical and keep your records clear.
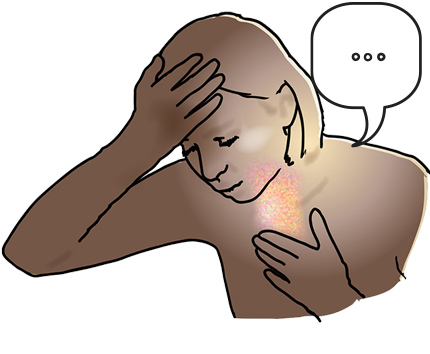
S = Subjective; what the patient tells you i.e. symptoms you cannot see such
as pain or how they are feeling, and vital details
about family or living conditions
O = Objective; what you can see i.e. signs such as heat, redness, range of
movement and what treatment you might give
such as which exercise, or how many and how often
A = Analysis: what you question may or may not be happening, so reasoning
through a problem such as progress the
patient is making comes in here
P = Plan: what you want to do next time, such as add a new treatment as
patient progresses
When you are ready, please proceed to the assessment of your patient.